Health equity is a growing concern around the world, especially as access to healthcare and other resources becomes more challenging for low-income individuals. Many factors can contribute to unequal access to healthcare, but one of the most important is social determinants of health (SDOH). Those conditions in the environment that have a direct impact on individuals and populations are referred to as SDOH. These conditions could include income levels, housing stability, education attainment, and access to healthy food. So why do we need to focus on SDOH? Understanding how these social factors influence overall wellbeing can go a long way toward ensuring everyone in our society has equitable opportunities—regardless of their background or socioeconomic context.
What is SDOH, and how does it impact population health?
The social determinants of health (SDOH) are the factors outside the medical system that influence health outcomes, including socioeconomic status, education, residential location, living conditions, employment, and access to health care. They also include the circumstances people are born into, grow up in, work in, live in, and age in. SDOH conditions can be both positive and negative. For example, a positive social determinant of health would be access to nutritious food. A negative social determinant of health would be exposed to harmful toxins. And while some SDOHs—such as exposure to toxins—are beyond an individual’s control, others—like access to nutritious food—are not.
SDOH is a significant factor in health inequalities within and between countries. Socioeconomic status directly affects health and sickness across nations of all income levels. According to the World health organization (WHO):
- Those born in high human development (HD) countries have 19 years more life expectancy than low HD nations.
- The low-educated report poor health 100% more often than the tertiary educated.
- The under-5 mortality rate in Africa is eight times higher than in Europe.
- Low- and middle-income countries accounted for most of the 15 million premature deaths in 2016 due to non-communicable diseases.
Several studies have shown that social determinants of health significantly impact population health outcomes, such as life expectancy, infant mortality, access to healthcare services, quality of care received, mental health status, and overall wellbeing. People from disadvantaged backgrounds, for example, often don’t have access to healthy food or suitable living conditions resulting in chronic illnesses. Further, people with low educational attainment may be unable to find jobs with good wages or affordable housing, resulting in unhealthy living conditions. Therefore, promoting healthy choices to eliminate these and other health disparities is not enough. Instead, public health organizations and their partners in industries like education, transportation, and housing must make improvements to the conditions in people’s settings.
SDOH has become increasingly important as the healthcare industry evolves towards providing value-based care to achieve greater health equity across populations. Healthcare providers now realize that to get the best overall outcomes, SDOH must be considered when providing treatment and making a difference in people’s lives.
Addressing social determinants of health to support equity
Addressing social determinants is essential for promoting equity among populations. To do this effectively, policymakers must employ a multi-sectoral approach when designing interventions that target SDOH at multiple levels, including individual, organizational, community, state, and federal levels. Some examples include increasing access to healthcare services through expanding Medicaid eligibility requirements; creating job training programs for low-income individuals; implementing nutrition assistance programs (like WIC or SNAP benefits); providing free school lunches for children from low-income families; creating tax credits for families with children living below the poverty line; increasing funding for public transportation initiatives; investing in community development projects such as affordable housing developments or community gardens; creating smoke-free zones near schools or childcare centers; etc. All these initiatives have successfully reduced disparities related to social determinants while promoting overall population health outcomes among underserved communities.
Examples of interventions to address social determinants of health
SDOH, or social determinants of health, can drastically impact the health of an entire community. Recognizing SDOH and taking action to address it are key ingredients in achieving health equity and promoting value-based care. Two examples demonstrating successful interventions to address SDOH are the Buckhead Community’s efforts to reduce violent crime in Atlanta and New York City’s Green Carts Initiative. By enforcing liquor laws and cutting down on alcohol outlet density, the Buckhead community improved safety and security. Similarly, the Green Carts Initiative enabled underserved neighborhoods to gain better access to fresh fruits and vegetables.
SDOH interventions are integral in promoting health equity and value-based care. They have been successful in making a difference in many communities around the world, yielding positive results for improved community health.
Implications for public policy
Public policies can help promote health equity in communities. So, in what ways can this be accomplished? Here are some possible solutions.
- National Framework: Establish a national social determinant of health framework with shared goals and responsibilities for identifying and addressing socioeconomic needs
- Data Standards: Standardize social determinants data across states to facilitate data aggregation and analysis towards common evaluation metrics to improve equity and reduce disparities
- Data Collection: Provide health insurance companies with sociodemographic information during enrollment to reduce inequities and improve communication and services.
- Cross-Sector Data Exchange: Create a modern data exchange infrastructure to facilitate data sharing between cross-sector partners.
- Research Funding: Invest in social determinants of health research so you can scale up effective interventions, programs and quantify the costs.
- Risk Adjustment: Enhance risk adjustment methodologies by incorporating social risk factors.
Social determinants of health (SDOH) are instrumental in reducing health inequity. By addressing SDOH through initiatives like value-based care, we can take meaningful steps toward providing equal and accessible healthcare for populations who need it most. We must recognize SDOH and its role in determining an individual’s well-being. With greater awareness and accountability for SDOH, we can create a more equitable and sustainable healthcare system that addresses gaps in both quality of care and access to care.
Achieving health equity and addressing social determinants of health is only possible through shared values, leadership, research, collaboration, and awareness.
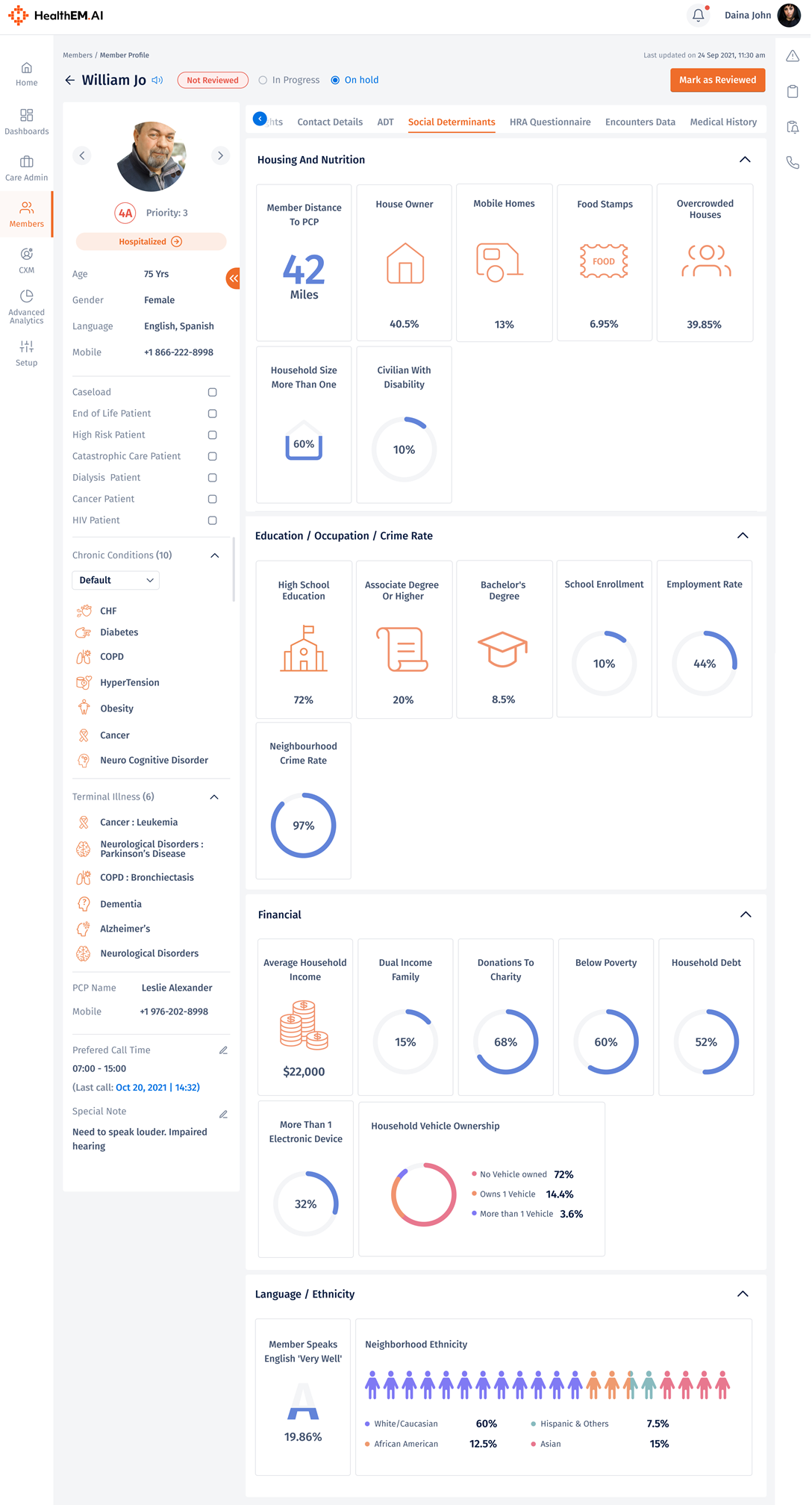
Here is how HealthEM.AI uses SDOH risk stratification in Total Care Management
Case example: Emma, the client’s social worker, received a referral for a patient named Ava from a care manager using the HealthEM risk stratification list. Ava did not want to remain in her mobile home as she had several complaints about where she lived. Emma spent some time with her to discuss the situation. During the conversations, Ava told Emma about a traumatic incident that she had never disclosed to anyone. Her life has taken on new meaning as Ava has been attending the senior center per the social worker’s guidance. Now that Ava feels supported, she looks forward to Emma’s visits. In an emergency, Ava knows to contact Emma. A therapeutic approach has successfully been established.